Abstract
Therapy-related acute lymphoblastic leukemia (t-ALL) is an emerging entity that encompasses cases of ALL that develop after prior exposure to cytotoxic therapy. We retrospectively reviewed all consecutive cases of adult ALL treated at City of Hope between 2000 and 2017 in order to identify cases of t-ALL. We defined t-ALL defined as ALL that occurred after prior exposure to chemotherapy and/or radiation and/or immunomodulatory agents. We excluded cases of ALL preceded by malignancy but without exposure to cytotoxic therapy. We compared t-ALL cases with de novo ALL cases treated during the same period to identify distinctive features.
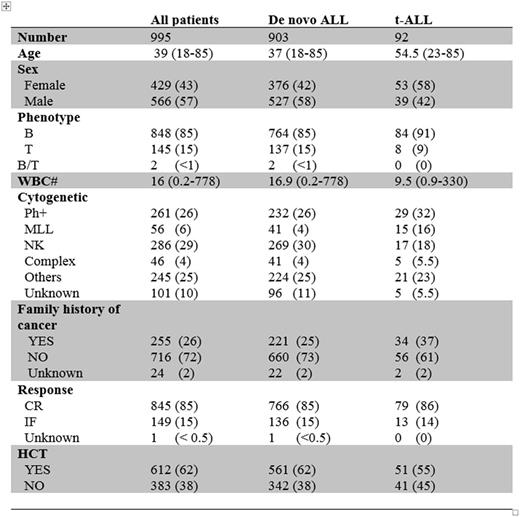
We identified 92 cases of t-ALL among 995 cases treated representing 9% of all adult ALL. The median age for t-ALL patients was 55 (23-85) yrs old, and the median latency for developing ALL was 6.6 (0.8-50.7) yrs from the time of original malignancy/disease diagnosis. Prior diagnosis was solid cancer in 50 (54%), hematological cancer in 34 (37%), combination of solid/blood caner in 2 (2%), and benign disease in 6 (7%) patients. Breast cancer was the most common prior diagnosis (N = 21), and this was followed by non-Hodgkin's lymphoma and multiple myeloma (13 cases each). 34 (37%) patients had prior chemotherapy only, 25 (27%) had prior radiotherapy only, 31 (34%) had prior combination of chemo-radiation, 17 (18%) received prior autologous transplant, and 15 (16%) had immunomodulatory agents. 2 cases of t-ALL were preceded by MDS. Phenotype was precursor B-cell in 84 (91%) patients. The latency interval from original diagnosis to ALL onset was shorter in patients carrying MLL gene rearrangement compared to patients carrying Philadelphia chromosome (Ph+) or other cytogenetic subgroups (2.4 yrs vs. 6.6 yrs vs. 7.3 yrs, p < 0.01), respectively, but there was no difference in latency based on type of cytotoxic therapy or prior diagnosis. Neither prior therapy, cytogenetic subgroup nor prior diagnosis influenced OS for t-ALL patients.
When compared to de novo ALL, t-ALL patients were older (55 yrs vs. 37 yrs, p <0.01) with more female predominance (58% vs. 42%, <0.01), but there was no difference in initial WBC or leukemia phenotype. t-ALL cases were associated with more frequent Ph+ (32% vs. 26%) and MLL rearrangement (16% vs. 5%) but less normal karyotype (18% vs. 30%) when compared to de novo ALL (p<0.01). Patients with t-ALL more frequently reported immediate family history of malignancy (37% vs. 25%, p=0.01). CR rate was similar for t-ALL and de novo ALL (p=0.88) and the rate of HCT utilization during ALL therapy was not different (55% vs. 62%, p=0.22). However, 1-yr OS was inferior in t-ALL compared to de novo ALL cases (76% vs. 87%, p<0.01).
In conclusion, we report the largest experience of t-ALL that restricts analysis to only cases with prior exposure to cytotoxic therapy. t-ALL was associated with unique features such as high frequency of Ph+ and MLL rearrangement as well as older age and female predominance. The latency period was shorter for patients carrying MLL gene rearrangement, similar to t-AML. Although CR rate and HCT utilization were similar for t-ALL and de novo ALL, OS was inferior for t-ALL patients. Molecular studies are warranted to further define t-ALL and determine if it has distinct genotypic features, and possibly differentiate it from de novo ALL that occurs coincidently in patients with prior chemotherapy exposure.
Salhotra: Kadmon: Consultancy. Khaled: City of Hope: Research Funding; Daiichi Sankyo, Inc: Other: Travel Support. Krishnan: Sutro: Consultancy; Onyx: Speakers Bureau; Takeda: Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Celgene: Consultancy, Equity Ownership, Speakers Bureau. Stein: Stemline: Consultancy; Amgen: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal